Inside Labs
Inside Labs
New Study Explores Lifestyle Habits That Can Keep Patients with COPD Less Exposed to Particulate Matter
Update 22.12.2022
Scientists find links between simple behaviors and lower levels of particulate matter, paving the way to practical guidelines for vulnerable people
Particulate
matter (PM) is a widespread type of air pollutant that negatively affects our
health. However, there is not much evidence backing up the current guidelines
for reducing one’s exposure to PM. In a recent study, researchers tackled this
problem by identifying various lifestyle habits linked to lower indoor PM
concentrations, and therefore lower PM exposure. Their findings could help
improve the quality of life of people with chronic respiratory diseases.
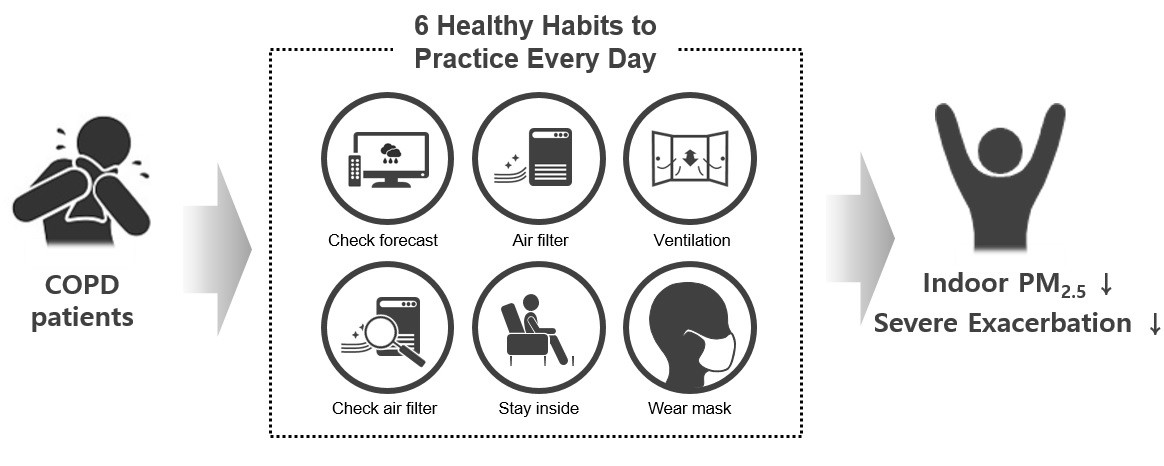
Certain lifestyle habits, such as checking the air filter regularly and
ventilating houses by opening windows, can reduce the indoor concentration of
particulate matter and prevent the unnecessary exposure of patients with
chronic obstructive pulmonary disorder to this air pollutant, researchers from
Korea say in a new study.
Photo courtesy: Sei Won Lee from University of Ulsan College of
Medicine
Over the past few decades, industrialization and an
excessive reliance on fossil fuels have greatly degraded the quality of the air
we breathe. Today, we know that several types of air pollutants, such as
nitrogen oxides and sulfur dioxide, deteriorate our overall health and can
cause or worsen many diseases. Aside from these specific compounds, particulate
matter (PM) constitutes another type of widespread air pollutant; one that can
unfortunately affect us during every stage of our lives.
Researchers have demonstrated that high concentrations
of PM—the assorted mixture of small solid particles and liquid droplets
suspended in air—impair proper lung development and can even lead to
respiratory problems in adulthood, such as chronic obstructive pulmonary
disease (COPD). Particles smaller than 2.5 micrometers (PM2.5),
about 30 times smaller than the diameter of a human hair, are especially
dangerous because they can easily travel deep into the lungs.
Of course, since we are still a long shot from
reducing the overall air pollution in the world to acceptable levels, the only
option we currently have is to protect ourselves from PM2.5 by minimizing
our exposure. However, most of the available lifestyle guidelines for avoiding
PM2.5 are based on experts’ opinions instead of actual scientific
evidence.
To help address this glaring issue, a team of
scientists led by Associate Professor Sei Won Lee of University of Ulsan
College of Medicine, Korea, recently conducted a study to find links between
indoor and outdoor PM2.5 exposure, lifestyle habits, and the
exacerbation (“flare-ups”) of symptoms in COPD patients. This work was published in Environmental
Research and supported
by the Research of Korea Centers for Disease Control and Prevention [No.
2019ER671100 and 01].
To address their research
question, the team enrolled 104 adults with COPD from four representative areas
of Korea, covering metropolitan, industrialized, and rural landscapes. Each
participant had to answer a questionnaire about their adherence to 20 daily
practices meant to avoid exposure to PM. Other questionnaires covered factors
that could affect indoor and outdoor PM concentrations, such as nearby traffic
volume and whether their home had a ventilation system or air filter installed.
Additionally, each participant had to place a sensor in their home that
measured indoor PM2.5 concentration. Finally, instances of COPD flare-ups
for each patient were checked monthly. “By analyzing all this information, we aimed to
elucidate the type of behaviors or habits that can effectively reduce indoor PM
concentration, as well as the impact of PM2.5 concentration on COPD
exacerbation,”
explains Dr. Lee.
After conducting
statistical analyses, the research team identified multiple lifestyle habits
that were linked to reduced indoor PM2.5 concentrations. Some
examples are checking air filters regularly, ventilating the home by opening
windows, operating air filters, and checking air-quality forecasts daily. Moreover,
the scientists showed that participants were more prone to severe COPD
exacerbation if exposed to higher PM2.5 concentrations for a long
period of time.
Taken together, the findings
of this study could serve as the basis for new, evidence-based guidelines for
reducing exposure to PM2.5, especially among those who are already
more vulnerable to it. “We believe that the quality of life of COPD patients
could be improved in the long term if they adhere to the daily practice of
those habits that, as we showed, can significantly reduce indoor PM
concentration,”
concludes Dr. Lee.
Let us hope this study
raises awareness of the problem of PM and arms people with simple, yet
effective, tools to reduce their PM2.5 exposure, ultimately
improving their overall health.
Reference
|
Authors
Title of original paper
Journal |
Hajeong Kim1, Geunjoo Na2,
Shinhee Park3, Seung Won Ra4, Sung-Yoon Kang5,
Ho Cheol Kim1, Hwan-Cheol Kim2, Sei Won Lee1 The impact of life behavior and environment on
particulate matter in chronic obstructive pulmonary disease Environmental
Research |
|
|
|
|
DOI
Affiliations |
10.1016/j.envres.2021.111265
1Department
of Pulmonary and Critical Care Medicine, University of Ulsan College of
Medicine, Asan Medical Center 2Department
of Occupational and Environmental Medicine, College of Medicine, Inha
University 3Department
of Pulmonary, Allergy and Critical Care Medicine, Gangneung Asan Hospital 4Division
of Pulmonary and Critical Care Medicine, Department of Internal Medicine,
Ulsan University Hospital, University of Ulsan College of Medicine 5Department
of Internal Medicine, Gachon University Gil Medical Center |
About National Institute of Health in Korea
The Korea National Institute of Health (KNIH), one
of the major operating components of the Ministry of Health and Welfare, leads
the nation’s medical research. Over the past seven decades, the KNIH has made
unwavering efforts to enhance the public’s health and innovate biomedical
research. The KNIH seeks to eradicate diseases and make people healthier. The
KNIH establishes a scientific basis and evidence underlying health policy as
well as provides national research infrastructures. We also promote public
health research. To this end, we make efforts to enrich a health research
environment by granting funds to research projects and keeping our resources,
data, and facilities more open and accessible to researchers.
Website:
http://www.nih.go.kr/NIH_ENG/
About Associate Professor Sei
Won Lee
Sei Won Lee is an Associate Professor of Pulmonology and Critical Care
Medicine, Asthma Center, and Lung Cancer Center at the Asan Medical Center,
University of Ulsan College of Medicine, Seoul, Korea. He mainly treats chronic
obstructive pulmonary disease (COPD), emphysema, and asthma. In addition to pharmacologic
treatments, he provides non-pharmacologic treatments, such as pulmonary
rehabilitation, bronchoscopic lung volume reduction, and bronchial
thermoplasty. His major research interests include microbiomes, particulate
matter, and pulmonary rehabilitation in chronic respiratory diseases. He
completed his residentship and fellowship at Seoul National University Hospital
and received an MD PhD degree from Seoul National University, Korea.

