Inside Labs
Inside Labs
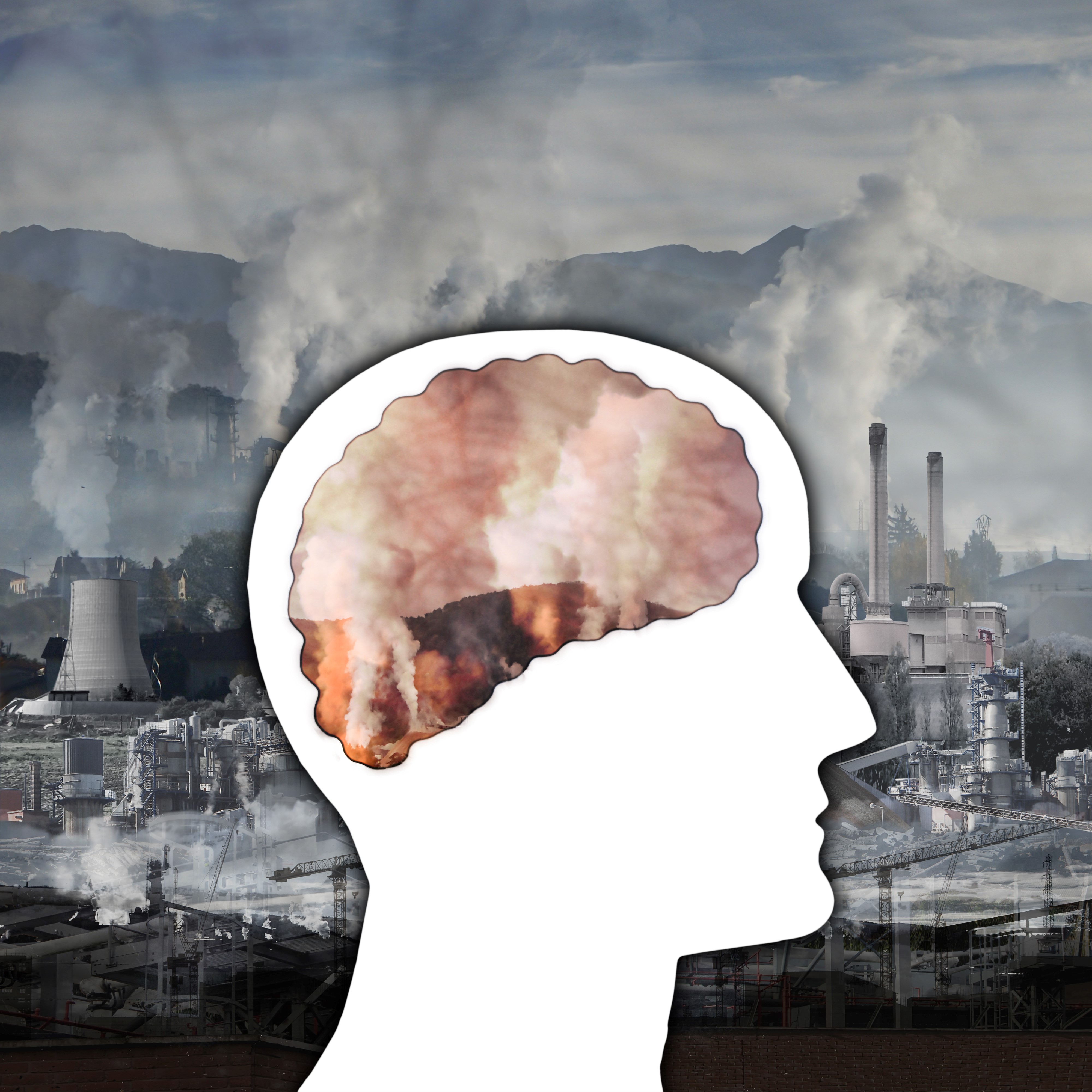
Air Pollution Can Harm Blood Vessels in the Brain, Says New Study by Korea National Institute of Health
Update 22.12.2022
The study finds that even low concentrations of particulate matter can damage the brain’s blood vessels, eventually causing neurological impairments
Particulate
matter (PM) exposure is a known risk factor for respiratory diseases. However, a
new study by Korea National Institute of Health shows that PM can also impair
the functioning of blood vessels in the brain, increasing the risk of neurodegenerative
diseases. The inflammatory molecular pathways that contribute to such dysfunction
are also revealed, paving the way for new strategies for preventing and
treating neurodegenerative conditions aggravated by PM, and combating this
public health threat.
The link between air
pollution and cerebrovascular diseases is becoming increasingly clear, making
particulate matter exposure an even greater threat to public health. Scientists
from KNIH have found that even low concentrations of particulate matter can
harm brain vascular health.
Photo courtesy: Shutterstock
Air pollution caused by particulate matter (PM) is a global health threat
and has been linked to several diseases of the respiratory system. However,
recent evidence shows that PM is also a risk factor for cerebrovascular diseases,
a group of conditions that affect blood flow and blood vessels in the brain.
Unfortunately, efforts to mitigate the neurological effects of PM have been
hindered by our poor understanding of the mechanisms via which PM damages the brain’s
blood vessels.
To overcome this roadblock, a team of researchers from the Korea National
Institute of Health (KNIH) examined how PM impairs the function of endothelial
cells, which constitute the inner lining of blood vessels and are an important
part of the blood-brain barrier (BBB). Their study, which was supported by funds (2017-NI62002-00 and 2020-NI-024-00) from
Research of Korea Centers for Disease Control and Prevention, was published online in Archives of Toxicology on 7th November 2020, and in print in February 2021.
The team, involving Dr. Jung Hyun Park, a researcher at KNIH, uncovered the
molecular mechanisms of PM-induced endothelial dysfunction. More importantly,
they found that even low concentrations of PM that do not cause cell damage are
sufficient to impair the integrity of blood vessels in the brain. Dr. Park
feels that this is a risky proposition. “Air pollution is not just an
environmental problem but has become a serious public health concern and a
social issue. What we are doing is researching how these factors will affect
people,” he says.
The NIH group used an in vitro cellular model—human brain
microvascular endothelial cells (HBMECs)—to study the effects of PM smaller
than 10 μm in diameter. First, they treated HBMECs with this PM, then used two
techniques—immunostaining and western blotting—to examine any protein-level changes
in the treated cells. Interestingly, they found that exposure to PM caused the
disruption of “junction proteins,” which are responsible for anchoring
endothelial cells to each other and preventing any gaps between them. This
implied that endothelial cells exposed to PM would be unable to prevent small
toxic molecules in the blood from leaking into the brain, potentially causing
neurological damage.
Next, the researchers set out to understand the molecular pathways through
which PM causes endothelial dysfunction. Given the known association between
inflammation and endothelial dysfunction, they tested whether PM caused
inflammation in the brain. Their findings showed that when cells were exposed
to PM, the cleavage of the protein Notch1, an important regulator of cell
signaling, increased. This, in turn, led to an increase in the levels of NICD—a
peptide released after Notch1 cleavage—that plays an important role in the
inflammatory process. Additional experiments showed that the PM-induced Notch1
and NICD signaling promoted both inflammation and cellular aging in HBMECs,
leading to endothelial dysfunction. These findings provided tangible evidence
for the possible mediators of PM-induced cerebrovascular disease.
Finally, in an attempt to uncover the therapeutic potential of their
findings, the research team investigated how Notch1 silencing affects
endothelial cells under conditions of PM exposure. They found that when Notch1
signaling is blocked, inflammation and cellular aging are inhibited. Therefore,
targeting Notch1 and NICD could prevent endothelial dysfunction even in the
presence of PM.
Summarizing the importance of their study, Dr. Park candidly explains, “Our
findings highlight the neurological risks associated with PM. They call for
urgent attention from both policymakers and the public in combatting this
threat and ensuring safe environments for all citizens. Even more importantly,
they open a new door for therapies that can help in preventing and managing
PM-related cerebrovascular disorders.”
Reference
|
Authors
Title of original paper
Journal |
Jung Hyun Park,
Ji‐Young Choi, Hye‐Kyung Lee, Chulman Jo, Young Ho Koh
Notch1‐mediated
inflammation is associated with endothelial dysfunction in human brain
microvascular endothelial cells upon particulate matter exposure
Archives
of Toxicology |
|
|
|
|
DOI
Affiliations |
10.1007/s00204-020-02942-9
Division of Brain
Disease Research, Department of Chronic Disease Convergence Research, Korea National
Institute of Health, 187 Osongsaengmyeong2(i)-ro, Osong-eup, Heungdeok-gu,
Cheongju-si, Chungcheongbuk-do 28159, Republic of Korea |
About National Institute of Health in Korea
The Korea National Institute of Health (KNIH), one
of the major operating components of the Ministry of Health and Welfare, leads
the nation’s medical research. Over the past seven decades, the KNIH has made
unwavering efforts to enhance the public’s health and innovate biomedical
research. The KNIH seeks to eradicate diseases and make people healthier. The
KNIH establishes a scientific basis and evidence underlying health policy as
well as provides national research infrastructures. We also promote public
health research. To this end, we make efforts to enrich a health research
environment by granting funds to research projects and keeping our resources,
data, and facilities more open and accessible to researchers.
Website:
http://www.nih.go.kr/NIH_ENG/
About Dr. Jung Hyun Park
Dr. Jung Hyun Park is a researcher in the Division
of Brain Disease Research at the Korea National Institute of Health. He obtained
his Bachelor of Science and Master of Biotechnology degrees at Kyungpook
National University, and received a PhD in Food Biotechnology from Korea
University. He joined the NIH in 2018, and has since focused his research on brain
diseases, examining the linkage between various external (environmental)
factors and degenerative brain diseases as well as the underlying risk factors.

