Antimicrobial Resistant Organism
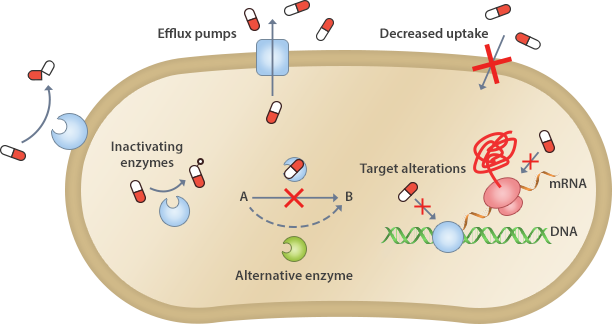
AMR mechanisms are largely classified into two types: (1) to prevent antimicrobials from reaching their target at sufficient concentrations or (2) to modify or bypass the targets on which the antimicrobials act.
Beta-lactamases produced by resistant organisms decompose antimicrobials by hydrolyzing the lactam ring.
Antimicrobials target bacteria-specific enzymes and/or organs, which means, the bacteria would become resistant when the target is modified. For example, some bacteria are resistant by modifying the penicillin-binding proteins that penicillin binds to, and others by modifying the rRNAs to prevent erythromycin and chloramphenicol from binding to ribosomes.
The decreased membrane permeability of bacteria prevents antimicrobials from entering the bacterial cytoplasm, and leads antimicrobial resistance (a mechanism mostly seen in multidrug resistant organisms).
The upregulated efflux pump releases antimicrobials such as tetracyclines, macrolides, and fluoroquinolones from the bacterial cells, causing antimicrobial resistance (a mechanism mostly seen in multidrug resistant organisms).
Some AMR bacteria do not require the biosynthesis of folic acid by modifying the metabolic process so that they can intake folic acid. Therefore, these bacteria exhibit a resistance phenotype to sulfa-based antimicrobials that prevent folic acid biosynthesis.
There are a variety of strains, the antimicrobial resistance of which is a serious problem in community infections and healthcare-related infections. The World Health Organization (WHO) promotes the Global Antimicrobial Resistance Surveillance System (GLASS). Korea has also designed eight sentinel hospital-based monitoring system for eight important AMR pathogens. In addition, the following six types of resistant bacteria, which are a risk factor for healthcare-associated infections, are designated as legal communicable diseases.
Staphylococcus aureus is an important causative pathogen of pneumonia, bacteremia, endocarditis, and surgical site infection. Since the late 1970s, the frequency of MRSA has increased worldwide with the emergence of new strains in the UK and Australia.
Vancomycin, a glycopeptide antimicrobial, has been considered for the treatment of MRSA infection. Vancomycin-intermediate S. aureus (VISA) was reported in Japan in 1996, and VRSA has gradually increased since the first report from USA in 2002.
Enterococci are commensal in the skin, mucous membrane, and gastrointestinal tract; therefore, it is necessary to distinguish infection from simple colonization. The most common species causing human disease are E. faecalis and E. faecium. Generally, enterococci exhibit resistance to many antimicrobials, including penicillin and cephalosporins, and there are limited treatment options for VRE infection.
MRPA is one of the most important multidrug-resistant pathogens for healthcare-associated infections causing pneumonia, bacteremia, and urinary tract infection. Combination therapy is recommended to treat MRPA infections because a synergistic effect between antibacterial agents with different mechanisms is expected.
MRAB is one of the important multidrug-resistant pathogens for healthcare-associated infections and is rapidly spread in the hospital environment.
Carbapenems have generally been considered as one of the last resorts to treat Gram-negative bacterial infections, but recently, resistance has often been reported. CRE can be classified into two groups: 1) carbapenemase-producing Enterobacteriaceae, and 2) carbapenemase-non-producing carbapenem-resistant Enterobacteriaceae. Of note, CPE is a clinical issue since the carbapenemase genes are able to transfer horizontally.